V0200A02A CAA-Cognitive loss/dementia: triggered, Step-by-Step
Step-by-Step Coding Guide for Item Set V0200A02A: CAA - Cognitive Loss/Dementia: Triggered
1. Review of Medical Records
- Objective: Ensure accurate documentation of cognitive assessments and any indicators of cognitive loss or dementia.
- Actions:
- Review the resident’s medical records, particularly focusing on cognitive assessments, physician notes, and previous MDS assessments.
- Look for any signs or symptoms documented in the last assessment period that indicate cognitive decline or dementia.
- Ensure that all relevant data from interdisciplinary team members has been considered in the assessment.
2. Understanding Definitions
- V0200A02A: CAA - Cognitive Loss/Dementia: Triggered: This item is marked when the Care Area Assessment (CAA) process identifies cognitive loss or dementia as a significant concern requiring further review and possible care planning.
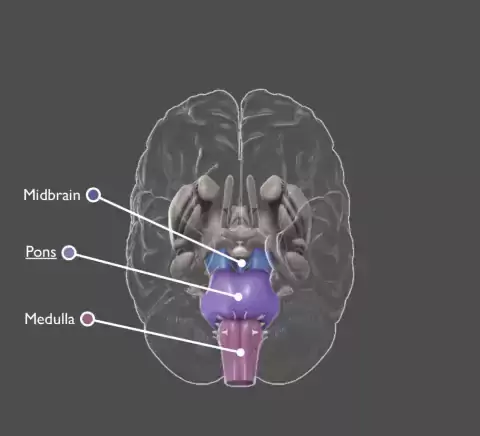
- Cognitive Loss/Dementia: Refers to the decline in memory, thinking, and reasoning skills that can affect a person's ability to perform daily activities. This includes conditions such as Alzheimer’s disease, vascular dementia, and other related disorders.
3. Coding Instructions
- Step-by-Step:
- Step 1: Review cognitive assessment data, including results from tools like the Brief Interview for Mental Status (BIMS) or the Staff Assessment for Mental Status.
- Step 2: Determine if the CAA has identified cognitive loss or dementia as an area that needs further attention. This is typically triggered by scores indicating moderate to severe cognitive impairment.
- Step 3: If cognitive loss or dementia is triggered, mark V0200A02A as "Triggered."
- Step 4: Document the rationale for triggering this item, including any observed changes in the resident’s cognitive status and how these changes impact their daily functioning.
4. Coding Tips
- Comprehensive Review: Ensure that the cognitive assessment considers all potential contributing factors, such as delirium, medication side effects, and acute illness, to avoid mislabeling dementia.
- Consistency: Cross-check findings with other parts of the MDS to ensure consistency across the assessment.
- Collaboration: Involve the interdisciplinary team, including physicians, nurses, and social workers, in the review process to get a holistic understanding of the resident’s cognitive status.
5. Documentation
- Objective: Maintain clear and detailed documentation supporting the decision to trigger the CAA for cognitive loss or dementia.
- Actions:
- Record all cognitive assessments that led to the triggering of this item.
- Document any discussions with the resident’s family or care team regarding changes in cognitive status.
- Ensure the care plan reflects any interventions or strategies developed in response to the triggered CAA.
6. Common Errors to Avoid
- Overlooking Acute Conditions: Do not mistake temporary cognitive impairment (such as delirium) for dementia without proper assessment.
- Inconsistent Documentation: Ensure that the rationale for triggering cognitive loss or dementia is documented consistently across all relevant sections of the MDS.
- Failing to Reassess: Regularly reassess the resident’s cognitive status to adjust the care plan as needed.
7. Practical Application
- Example 1: A resident scores poorly on the BIMS, showing severe cognitive impairment. This triggers V0200A02A, leading the care team to develop a plan that includes daily cognitive stimulation activities and regular monitoring for any changes in cognitive status.
- Example 2: A resident with moderate dementia begins to show signs of increased confusion and memory loss. After reviewing the medical records and recent assessments, the care team triggers V0200A02A and adjusts the care plan to include more structured daily routines and environmental modifications to support the resident’s cognitive function.
Please note that the information provided in this guide for MDS 3.0 Item set V0200A02A was originally based on the CMS's RAI Version 3.0 Manual, October 2023 edition. Every effort will be made to update it to the most current version. The MDS 3.0 Manual is typically updated every October. If there are no changes to the Item Set, there will be no changes to this guide. This guidance is intended to assist healthcare professionals, particularly new nurses or MDS coordinators, in understanding and applying the correct coding procedures for this specific item within MDS 3.0.
The guide is not a substitute for professional judgment or the facility’s policies. It is crucial to stay updated with any changes or updates in the MDS 3.0 manual or relevant CMS regulations. The guide does not cover all potential scenarios and should not be used as a sole resource for MDS 3.0 coding.
Additionally, this guide refrains from handling personal patient data and does not provide medical or legal advice. Users are responsible for ensuring compliance with all applicable laws and regulations in their respective practices.